Linda Laubenstein Award
About the Linda Laubenstein Award
An Award for HIV Clinical Excellence
The New York State Department of Health AIDS Institute established the Dr. Linda Laubenstein Annual HIV Clinical Excellence Award in 1992. The award honors those physicians who, beyond providing the highest quality of clinical care for people with HIV/AIDS, are also distinguished by their compassionate manner and their wholehearted involvement in the ongoing effort to achieve comprehensive care for persons with HIV/AIDS.
The award was created to recognize the doctors who were there early in the epidemic; to applaud those who are educating others about emerging changes in the available scientific research and clinical information about HIV/AIDS; to acknowledge those who have participated in the process of establishing medical standards for HIV care; and to commend those physicians who serve both as clinical leaders and as compassionate care providers with each individual patient. The Laubenstein Award represents an opportunity for the AIDS Institute to highlight the contributions of physicians or other clinicians whose record of service has been extraordinary and to publicly thank them for their accomplishments.
Linda Laubenstein, MD, 1947-1992
The HIV Clinical Excellence Award was established in memory of Dr. Laubenstein, a Manhattan physician, to honor her pioneering work and outstanding contribution to the quality of AIDS care in the early years of the epidemic. In 198l, Dr. Laubenstein treated many of the country’s first AIDS patients. With Dr. Alvin Friedman-Kien, she co-authored the first medical journal paper on the rapidly increasing incidence of Kaposi’s sarcoma among gay men and, in 1983, organized the first large medical conference on AIDS. Although Dr. Laubenstein used a wheelchair from the age of 5 as a result of childhood polio and severe asthma, she devoted most of her private practice to her own exemplary brand of AIDS care, making house calls and emergency room visits at any hour, speaking out to urge social organizations and government to respond to the AIDS epidemic, and founding an organization to employ AIDS patients.
About the AIDS Institute
Created in 1983 by legislative mandate to coordinate New York State’s response to the HIV/AIDS epidemic, the New York State Department of Health AIDS Institute strives to prevent HIV infection and improve the quality of life of those infected and affected by HIV. Toward that end, the Institute focuses on insuring that people with HIV/AIDS receive high quality health care and supportive services. The AIDS Institute is committed to assuring that there is ongoing development of the health care infrastructure so that people with HIV/AIDS have access to a coordinated system of health care and services including access to clinicians with expertise in HIV care and state-of-the-art treatment guidelines. In keeping with these goals and principles, the AIDS Institute is pleased to continue its tradition of presentation of the Dr. Linda Laubenstein Annual HIV Clinical Excellence Award to those clinicians who have made unparalleled contributions to HIV care and prevention.
2018-present Awardees
2021
Joseph P. McGowan, MD
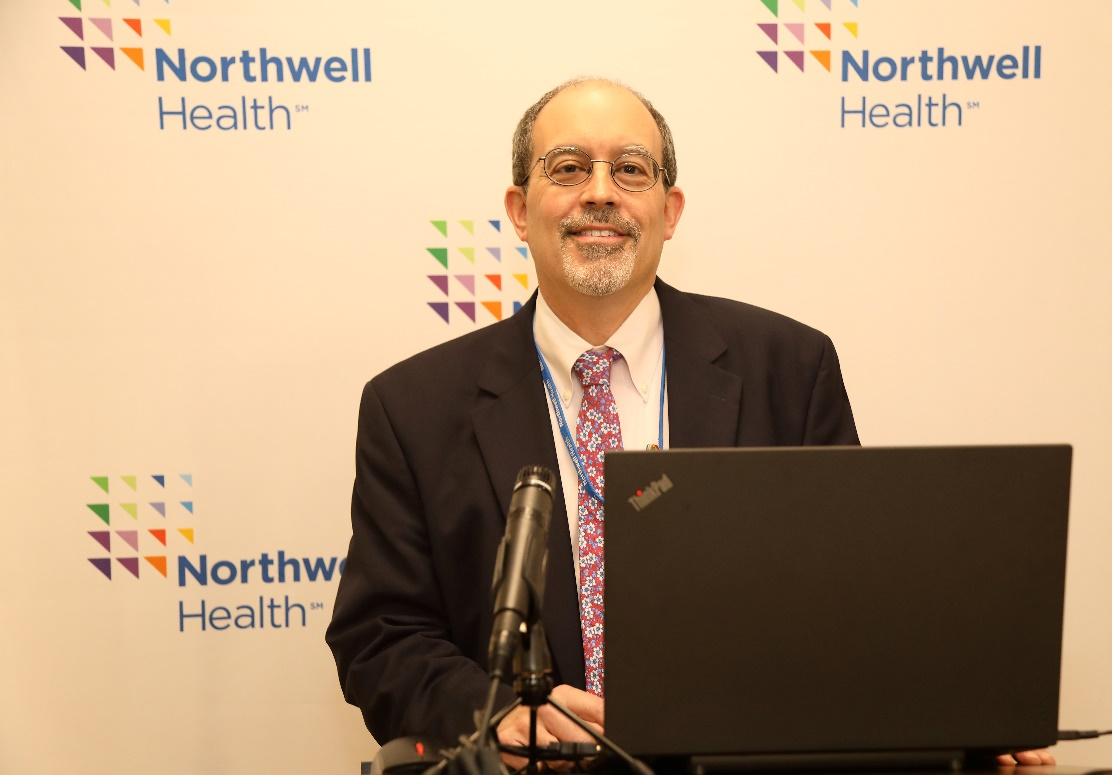
With the 29th annual Linda Laubenstein award we recognize a clinician for his leadership and unwavering commitment to providing clinical care that has profoundly expanded awareness and access to HIV medicine and prevention in New York State. It is a great pleasure to recognize Dr. Joseph McGowan as this year’s Linda Laubenstein awardee.
Among his many roles, Joseph P. McGowan, MD, FACP, FIDSA is Professor of Medicine at the Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, Professor in the Center for Health Innovations and Outcomes Research at the Feinstein Institute for Medical Research and is on faculty at the Albert Einstein School of Medicine.
Dr. McGowan has been providing care to people with HIV for over 30 years, with many of those years serving in the South Bronx, an epicenter for the HIV epidemic in the US where many communities were challenged by poverty, language barriers, cultural barriers and educational barriers. There he saw HIV and AIDS as a truly opportunistic infection that targeted the most vulnerable populations in terms of access to care, the ability to negotiate complex medical systems, and eventually, treatment.
“I learned more from making home visits to my patients in the South Bronx than I could have ever learned in any classroom about what people with HIV have to deal with and the obstacles that must be overcome.” says Dr. McGowan. His understanding, empathy, and compassion for his patients is reflected in his approach to providing care, which includes convening a multidisciplinary team of nurses, social workers, health educators, peer navigators, and pharmacists to provide not only HIV treatment but patient education, assessment of medication access issues, mental health issues, substance use issues, housing challenges, and addressing social supports.
Beyond his work as a clinician board-certified in infectious diseases and credentialed by AAHIVM as an HIV Specialist, Dr. McGowan serves as administrator, researcher, educator, and grant writer. He has been involved in numerous HIV clinical trials for over 25 years, published over 60 original articles and abstracts on HIV and AIDS, and is currently the Principal Investigator on over a dozen grant funded programs to provide HIV primary care and prevention from the CDC, HRSA and New York State Department of Health. He is the Medical Director of the Center for AIDS Research & Treatment at the North Shore University Hospital on Long Island, NY and Director of the HIV Service Line Program for the Department of Medicine for Northwell Health, the largest provider of health care in New York. He also serves as the Medical Director of the AIDS Education and Training Regional Center at SUNY Stony Brook and provides invaluable leadership as Chair of the Medical Care Criteria Committee of the New York State AIDS Institute’s Clinical Guidelines Program, which establishes treatment guidelines for HIV management and prevention.
When asked what the most rewarding part of his job is, he says that it is without a doubt when he is in the room with his patient, door closed, discussing what is going on with them and, hopefully, supplying them with education and tools to motivate them to adopt and maintain healthy practices and get the most out of their treatments. As for the rest of what he does, being the best clinician he can be is most important to him. As he puts it, “…it informs everything else I do.”
For his passion, unique skills, and extensive experience; for his commitment to serving the HIV population; and for his contribution to the advancement of HIV primary care through his work as researcher, educator, writer, and most importantly dedicated clinician, we are delighted to recognize Dr. McGowan with the 2021 Linda Laubenstein award.
2020
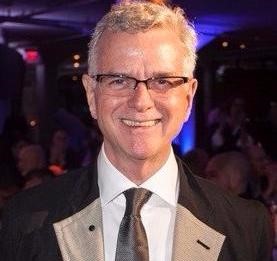
Jerome Ernst, MD

With the 28th annual Linda Laubenstein award we recognize a clinician for his leadership and unwavering commitment to providing clinical care that has profoundly expanded awareness and access to HIV medicine and prevention in New York State. It is a great pleasure to recognize Dr. Jerome Ernst as this year’s Linda Laubenstein awardee.
Dr. Jerome Ernst is an experienced provider, health plan leader, and researcher with over five decades of experience in the medical field. Dr. Ernst has dedicated his career to advancing the health of PLWH. He is currently the Chief Medical Officer of Amida Care, a community-sponsored, not-for-profit Medicaid Managed Care Special Needs Health Plan in New York City.
In the 1980s, Dr. Ernst created and served as the Medical Director of the AIDS Program at Bronx-Lebanon (now BronxCare), starting with one social worker and growing to a staff of over 30. Dr. Ernst created the AIDS Unit, the AIDS clinic and the AIDS research program, as well as attracted significant grant-funded programs in research and service to the Hospital. In 1989, Dr. Ernst was the Principal Investigator at Bronx-Lebanon for the CDC’s nationwide study looking at unknown HIV infection; new data about HIV risk was a major outcome of the study. Dr. Ernst has been a major contributor to the HIV literature via published articles, book chapters, and conference presentations throughout his career.
From 1999 – 2017, Dr. Ernst concurrently served as the Medical Director of the AIDS Community Research Initiative of America (ACRIA), a global leader and resource on HIV and aging, where he oversaw their portfolio of research studies, including clinical drug trials. Dr. Ernst served as the Associate Director of Medicine, Chief of the Division of Pulmonary Diseases, and Acting Chief of the Division of Infectious Diseases at Bronx-Lebanon Hospital Center. Dr. Ernst was also an Associate Professor of Medicine at Albert Einstein College of Medicine and is a Fellow of the New York Academy of Medicine and the American College of Chest Physicians.
Dr. Ernst was an early supporter of how managed care could work for PLWHA through a dedicated HIV Special Needs Plan (SNP). Creating AIDS managed care programs for Medicaid recipients was the subject of his Master’s Project (titled “AIDS Managed Care in New York State”) at New York University, where he received his MS degree in 1996. Dr. Ernst was instrumental in the SNP model’s development and continues to significantly contribute to its success.
Dr. Ernst provides invaluable support and guidance daily to the staff of Amida Care, New York State’s largest Special Needs Plan for PLWHA. Dr. Ernst has been instrumental in leading the Organization’s as well as State efforts to End the Epidemic and has used his decades of on-the-ground experience to guide and support Amida Care’s clinical, behavioral health, pharmaceutical, and administrative staff. Under his clinical leadership, Amida Care has developed and implemented successful initiatives to improve suppression, including the Ending the Epidemic Managed Care Organization pilot with the NYSDOH AIDS Institute and a viral load suppression incentive program.
For his passion, unique skills, and extensive experience; for his commitment to serving the HIV population; and for his contribution to public health efforts through the involvement of managed care models, we are delighted to recognize Dr. Ernst with the 2020 Linda Laubenstein award.
2019
Marguerite A. Urban, MD

With the 27th annual Linda Laubenstein award we recognize a clinician who, in addition to her outstanding contributions to the advancement of HIV clinical care, has consistently demonstrated her wholehearted commitment to the education of clinical providers and her compassion for the patients receiving their care. It is a great pleasure to recognize Dr. Marguerite A. Urban as this year’s Linda Laubenstein awardee.
Marguerite A. Urban, MD is Professor of Medicine in the Division of Infectious Diseases at the University of Rochester (UR) School of Medicine and Dentistry and the Medical Director for UR Center for Community Practice. Dr. Urban studied Chemistry at Villanova University and then went on to obtain her MD and complete a residency program in Internal Medicine at the Medical College of Pennsylvania.
Her first position after residency training was at the Philadelphia Department of Public Health STD clinic where she worked as a staff physician and was the Study Coordinator for a CDC sponsored clinical trial evaluating the management of HIV/syphilis co-infections. This experience prompted a lifelong interest in public health and especially STI/HIV care and prevention.
In 1991, she moved to Rochester to pursue a fellowship in Infectious Diseases at the University of Rochester and stayed on as a faculty member. Since that time, she has been the Principal Investigator (PI) for numerous state and federal projects focused on sexual health and HIV prevention. She has cared for patients living with HIV at the UR AIDS Center, served on HIV/STI related NYS AI committees, conducted research as a Co-Investigator for NIH funded clinical trials related to HIV/STI prevention, and provided extensive clinical education and training regarding sexual health, and HIV/STIs throughout New York and nationally. She currently directs the NYS Clinical Education Initiative (CEI) Sexual Health Center of Excellence and continues to serve as the Medical Director of the Monroe County STD Clinic (a position she has held since 1994).
2018
Dr. Antonio E. Urbina

Dr. Antonio E. Urbina received his joint BS/MD from the University of Florida’s Junior Honors Medical Program in Gainesville, Florida in 1992. He completed his residency in Internal Medicine at Saint Vincent Catholic Medical Center (SVCMC) in Manhattan in 1995. At that time, St. Vincent’s was the epicenter of New York City’s AIDS epidemic. It housed the first and largest AIDS ward on the east coast and was referred to as the “ground zero” of the AIDS epidemic. Dr. Urbina provided both outpatient and inpatient services to thousands of patients during that critical time in the HIV epidemic, including many young patients with advanced AIDS.
From 2003-2015, he served as the principal investigator (PI) of the HRSA-funded AIDS Education and Training Center (AETC) and New York State Department of Health (NYS DOH) AIDS Institute’s Clinical Education (CEI) grants at SVCMC and Mount Sinai St. Luke’s-Roosevelt Hospital. From 2015 until the present, Dr. Urbina has served as the PI for the NYS DOH AIDS Institute CEI’s HIV/HCV Center of Excellence at Mount Sinai Hospital. Under his leadership, he was able to provide HIV education to thousands of primary care and specialty clinicians throughout New York State. In 2005, he created the first multi-disciplinary workgroup at SVCMC that oversaw the care of HIV-positive pregnant women. This group brought together the divisions of HIV with OB/GYN, pediatrics, social work and nursing. As a result of this integrated care-team, perinatal transmissions at SVCMC dropped substantially. From 2007-2009, Dr. Urbina served on the Presidential Advisory Council on HIV/AIDS (PACHA) and more recently on Governor Cuomo’s Task Force to end the AIDS epidemic in NYS.
From 2003 until the present, Dr. Urbina has delivered hundreds of clinical trainings across New York State. These trainings have directly led to more patients being diagnosed, linked to HIV care, and initiated on antiretroviral therapy–thus contributing to the decreasing incidence of new HIV infections across NYS. Additionally, through the CEI Line and the tele-mentoring CEI HIV ECHO program, Dr. Urbina has provided individual and group technical assistance across hundreds of community health centers and institutions across NYS. Importantly, Dr. Urbina has been directly responsible for providing technical support in writing and implementing clinical care and quality improvement projects in emergency and primary care institutions throughout the country. One example of this was the successful implementation of an integrated emergency department and outpatient post exposure prophylaxis algorithm across both Mount Sinai St. Luke’s and Roosevelt Hospitals in New York City.
Dr. Urbina’s research has focused on HIV and has ranged from clinical trials to implementation science. He has been involved as PI in clinical trials looking at therapies for addressing HIV-associated body composition changes (lipodystrophy) as well as publishing on long term toxicities of antivirals. Dr. Urbina has served as PI on multiple Phase II and III HIV clinical trials. His research has also focused on the role that acute HIV infection plays in onward transmissions. As a result of an editorial that he co-authored in the New York Times, the New York City Department of Health and Mental Hygiene now implements pooled, viral load testing at various sexual health clinics across New York City. In 2004, Dr. Urbina published a land-mark article in CID that described the intersection of HIV and methamphetamine use, highlighting the medical and psychiatric complications.
Currently, Dr. Urbina is an Associate Professor of Medicine at the Icahn School of Medicine and serves as the Medical Director for the Mount Sinai Institute for Advanced Medicine’s Chelsea Clinic.
2012-2017 Awardees
2017
Bruce D. Agins, MD, MPH
Former Medical Director, NYSDOH AIDS Institute

The New York State Department of Health (NYSDOH) AIDS Institute (AI) established the Dr. Linda Laubenstein Annual HIV Clinical Excellence Award in 1992. Each year since, the AI has honored clinicians in New York State whose commitment to excellence carries on the standard set by Dr. Linda Laubenstein early in the AIDS epidemic as she provided compassionate care and dedicated advocacy for patients with HIV and conducted clinical research.
With the 25th annual Linda Laubenstein award, the AI recognized Dr. Bruce Agins. In addition to his outstanding contributions and influential leadership within the AIDS Institute, Dr. Agins, former Medical Director of the AI, consistently demonstrated his compassion and wholehearted commitment to caring for those affected by HIV.
Dr. Agins earned his bachelor’s degree in anthropology from Haverford College, his medical degree from Case Western Reserve University, and a master of public health degree from Columbia University. He served as the Director of AIDS programs in two New York hospitals in the 1980s before being appointed Assistant Medical Director of the NYSDOH AI in 1990. He became Medical Director in 1995 and served for 27 years before retiring in October 2017. Among his many other accomplishments during his tenure with the AI, Dr. Agins created an HIV guidelines program to assist New York State clinicians in providing evidence-based care; created state, national, and international quality programs to ensure delivery of high-quality care for people living with HIV in New York State and around the world; and involved consumers and ensured that their voices are heard in all aspects of policy and clinical care.
Dr. Agins has influenced countless clinicians, public health professionals, and members of the community with his tenacious pursuit of high-quality clinical care for underserved populations. He has consistently brought creativity, energy, and innovation to his work as a public health physician, clinical professor, mentor, and volunteer.
True to his enduring spirit of dedication to those affected by HIV, he will start a new chapter of his career with the University of California San Francisco, where he will continue to promote high-quality care for people living with HIV across the globe.
2016
James F. Braun, DO
James F. Braun, DO, received his medical degree from the Kansas City University of Medicine and Biosciences and completed an internship and residency in Family Medicine at the Michigan Osteopathic Medical Center in Detroit. Originally intending to practice as a primary care provider in a “small town,” he ultimately settled in Greenwich Village in the early 1980s, when the AIDS epidemic was first being recognized in New York City.
Dr. Braun was a clinician in the early days of the free Community Health Project and later established a private practice in the Village. Like Dr. Laubenstein, Dr. Braun made many house calls to patients who were too sick to come to his office. He joined other early leaders in the creation of the Safer Sex Committee of New York and coauthored the Gay Men’s Health Crisis publication Healthy Sex is Great Sex, which became the standard for safer sex guidelines thereafter. He served as a board member of the People With AIDS (PWA) Health Group and the Association of Physicians in AIDS Medicine (APAM), and as an Executive Committee member of the Forum for Collaborative HIV Research.
In 1990, Dr. Braun founded PRN, which will soon complete its 26th year of continuous monthly meetings, as a peer-support and education group for healthcare providers struggling to cope with the ever-changing needs of people living with HIV and AIDS. PRN is a respected educational resource for physicians seeking to learn about state-of-the-art science, clinical medicine, and policy issues on the forefront of HIV care. Through PRN, Dr. Braun is likely responsible for educating more private practitioners about HIV care than anyone else in New York State. Dr. Braun has been a key ally of the AIDS Institute Office of the Medical Director for many years, a partnership now solidified through his work with the Clinical Education Initiative (CEI).
In 2006, Dr. Braun served as vice-president on the founding board of directors for the American Conference for the Treatment of HIV (ACTHIV) and coined its name, and from 2007 on, Dr. Braun has served as vice-chair of the HIV, Hepatitis, and STI Advisory Panel for the Medical Society of the State of New York (MSSNY).
Dr. Braun has coauthored numerous scientific publications; as Program Director for the live meetings of PRN and Editor-in-Chief of The PRN Notebook and The PRN Notebook Online, he has spotlighted advances in the early diagnosis and management of HIV/AIDS and its complications. Since 2010, he has overseen the production of CEI’s online educational video programs for CME through PRN’s collaboration with the AIDS Institute. Dr. Braun remains strongly committed to increasing awareness of the management and prevention of HIV/AIDS, viral hepatitis, and their numerous complications in both general medicine as well as subspecialties.
Samuel T. Merrick, MD

Samuel T. Merrick, MD, earned his medical degree from the University of Virginia after spending 3 years as a software developer for a consulting startup. He completed his residency at The New York Hospital, serving as Assistant Chief Resident in his final year.
In 1991, Dr. Merrick joined the Center for Special Studies (CSS) at Weill Cornell Medical College, a comprehensive, multidisciplinary adult HIV clinic established as one of the early Designated AIDS Centers. He helped expand services in 1997 with the opening of a new clinic in Chelsea.
Dr. Merrick was an active participant in the AmFar Community Based Clinical Trials Network in the mid- to late-1990s, but his career has focused primarily on patient care and teaching. In 2001, Dr. Merrick was named Medical Director of CSS. Since that time, he has worked to preserve and maintain the original vision of ensuring true continuity of care between outpatient and inpatient settings and full communication among care team members through daily interdisciplinary rounds. In this continuity of care model, Dr. Merrick cares for many patients he first treated in the 1990s; the daughter of two of his early patients remains in care at CSS and just delivered healthy twins.
Currently an Associate Professor of Clinical Medicine at NYPH-WCMC, Dr. Merrick has been teaching at the bedside and in the clinic throughout his career. He has served for almost 10 years on the AIDS Institute Quality of Care Committee and applied his programming background in working with the HIVQUAL team to enhance and streamline data retrieval from the electronic medical record to further quality goals. He has also served for 9 years on the Medical Care Criteria Committee, the last 2 years as Chair, and has been the primary contributor to significant NYSDOH AIDS Institute guidelines, including acute infection, when to initiate treatment, initial ART regimens, PEP, and PrEP. Dr. Merrick’s guidance and contributions to the Clinical Guidelines Program have enhanced the quality of care for patients throughout the New York State.
Over the past few years, Dr. Merrick has played an active role in developing a broad coalition of partners through the Delivery System Reform Incentive Program (DSRIP) funding process, working with colleagues to form the REACH (Ready to End AIDS and Cure Hepatitis C) Collaborative, a joint project encompassing high-prevalence areas in New York City and offering a distinct array of services to populations at risk for or diagnosed with HIV or hepatitis C. The REACH Collaborative aims to set the standard for institutional-community cooperation in ending the epidemic.
Dr. Merrick is deeply grateful to the patients with whom he has worked for more than 25 years, who show him each day the true meaning of strength and perseverance.
2015
Robert Muriyama,MD, MPH
Chief Medical Officer, Apicha Community Health CenterDr Murayama has been Chief Medical Officer of Apicha Community Health Center, in lower Manhattan, since 2008. He helped transform Apicha Community Health Center from an HIV/AIDS service organization to a Federally designated health center (FQHC-LA) targeting the LGBT community, people living with HIV/AIDS and residents of the lower eastside of Manhattan. Under his leadership health services expanded to include HIV/AIDS Primary Care, Trans* Health and Wellness Clinic, Mental Health Services, LGBT Primary Care Clinic, Sexual Health Services and an Anal Cancer Prevention Program.
He serves on the New York State AIDS Institute HIV Quality Advisory Committee, New York State ADAP Medical Advisory Committee, Clinical Committee and HIV/AIDS subcommittee of the Community Health Care Association of NY State (CHCANYS), LGBT Primary Care Alliance of the National Association of Community Health Centers (NACHC), and the Public Policy Committee of the American Academy of HIV Medicine.
Dr Murayama is board certified in Internal Medicine and a graduate of the State University of New York at Syracuse School of Medicine and Columbia University Mailman School of Public Health. He is an Assistant Clinical Professor of Medicine at NYU School of Medicine.
Rona M. Vail, MD
HIV Specialist, Callen-Lorde Community Health CenterRona M. Vail, MD, is an American Academy of HIV Medicine (AAHIVM) certified specialist who has provided medical care to HIV-infected individuals since the beginning of the epidemic. She has been at the Callen-Lorde Community Health Center since 1999, where, in addition to providing patient care, she has also provided HIV education and training to community members, students, residents, and medical professionals, and has mentored new care providers. Dr. Vail serves on the New York State Department of Health AIDS Institute’s Medical Care Criteria Guideline Committee and the HIV Quality of Care Committee.
Dr. Vail first encountered patients living with HIV while she was in medical school, when the first unusual cases of pneumocystis pneumonia (PCP) were reported in gay men. After completing her medical residency, Dr. Vail served as Assistant Chief Physician for Riker’s Island Health Service, where she was responsible for coordinating the medical care of 2,500 inmates. In 1991, she became the Director of HIV Services at Gouverneur Hospital in lower Manhattan, where she oversaw an ambulatory HIV service providing comprehensive primary care for approximately 800 HIV-infected individuals. During her last two years at Gouverneur, she consulted on HIV for the New York City Health and Hospitals Corporation, the public hospital system of New York.
A desire to work closely with the LGBTQ community and others most in need led Dr. Vail to the Community Health Project in its grassroots days. For the past sixteen years, she has served thousands of patients as a Medical Director, a Clinical Director of HIV Services, and an HIV specialist at Callen-Lorde Community Health Center.
Dr. Vail is widely regarded for her exceptional care and for commitment to patients and the community:
“Dr. Vail has been my doctor for 12 years. She is the best doctor I’ve ever had, and I had a few, but not one could fill her shoes. I am the worst patient a doctor can have, but Dr. Vail has never given up on me. I am so grateful. She means the world to me. I can’t begin to imagine my life without her. My health, physically and mentally, depend on her. I feel that I could trust her, and feel safe, and know that she is always doing her best to keep me healthy and sane. I’m really blessed. I thank God for finding such a wonderful person to take care of me and keep me alive for another 12 years God willing.”
“Rona gives me the confidence to live my life normally.”
“Dr. Rona Vail is one of the very best doctors that I have known. She is very professional and kind. She puts patients at easy with her bedside manner and is acutely aware of new medical treatments. I HIGHLY recommend Dr. Vail!”
Beyond providing patient care, Dr. Vail has also served the community as a board member of God’s Love We Deliver (1994-99), as a member of numerous committees and advisory groups, and through participation in clinical research.
2014
HIV Clinical Guidelines Team
From Dr Bruce Agins : It is my honor and pleasure to present the 2014 Linda Laubenstein HIV Clinical Excellence Award – I haven’t been able to come to Albany for quite a few years to make the award, and have missed this opportunity which is one of the most enjoyable parts of my job. It is particularly fitting to take a moment and think about Linda Laubenstein this year as we – almost unbelievably – focus on ending an epidemic that began over 30 years ago at a time when few physicians stood up to the plate to take care of people who were dying of a mysterious, stigmatizing and potentially contagious illness. For those of us who remember this time, we can also draw parallels to our current struggles with Ebola and think of those who are taking risks by going to help provide care to people who are dying in throngs from yet another virus. Some of you may know about Linda Laubenstein from her fictional incarnation as Dr. Emma Brookner in The Normal Heart which captured her fierce commitment and passionate advocacy. Laubenstein was a Manhattan physician whose pioneering work and outstanding contribution to the quality of AIDS care in the early years of the epidemic was legendary.
In the early 1980s, Laubenstein treated many of the New York’s first AIDS patients. She co-authored the first medical journal publication on the rapidly increasing incidence of Kaposi’s Sarcoma among gay men, and co-founded an organization that hired people living with AIDS called “multitasking” so that they could work while they were living with their illness, otherwising facing insurmountable obstacles to getting jobs because of their illness and their disfiguring KS lesions. Although Dr. Laubenstein used a wheelchair from the age of 5 as the result of childhood polio and struggled with her own medical problems, she devoted most of her private practice to her own exemplary brand of AIDS care, making house calls and emergency room visits at any hour, speaking out to urge social organizations and government to respond to the AIDS epidemic. Dr. Laubenstein’s commitment was inspirational, and it is in her memory that we honor this year’s awardees, as we do each year.
Since 1992 the New York State Department of Health has awarded the Dr. Linda Laubenstein HIV Clinical Excellence Award in 1992 to physicians who, besides providing the highest quality of clinical care for people with HIV/AIDS, are also distinguished by their compassionate manner and their wholehearted involvement in the ongoing effort to achieve comprehensive care for persons with HIV/AIDS. The award has recognized doctors who were there early in the epidemic; those who have demonstrated innovative models of excellence in HIV care, those who have educated others about emerging changes in scientific knowledge and clinical information about HIV; participated in the process of establishing medical standards for HIV care, and above all those who have championed quality of care as both leaders and compassionate, caring physicians to their patients.
This year, we have broken with tradition by making an important exception to the practice of recognizing individuals. Underlying the work of each practitioner is a framework of clinical practice guidelines: recommendations and guidance that are developed by expert panels of practitioners, joined by consumers for the past decade, that establish basic standards and norms of practice. New York State sponsored the first HIV clinical guidelines program in the world – launched in the mid-1980s, supporting both adult and pediatric guidelines. Since the early days of the program which also included groundbreaking guidance to support practices of preventing mother-to-child transmission, it was the vision of Nick Rango and his medical team, led by Gary Burke, to sponsor a guidelines program. Guidelines were, in fact, a relatively new idea at that time and often met with resistance by physicians as cookbooks – to ensure that standards were in place to provide quality HIV care for patients with AIDS, many of whom were being hospitalized with strange infections, not well understood except by only a handful of specialists. In the early 1990s, as HIV care began to shift to the outpatient clinic, ambulatory care guidelines were needed, and almost miraculously, the first treatment guidelines when antiretroviral therapy became available. We have honored many chairs of our guidelines committees with the Laubenstein Award, and it became apparent that it was important to recognize the work behind the committees of physicians that has been directed and managed together with the Office of the Medical Director.
After two previous contractors, the Johns Hopkins University Division of Infectious Diseases under the leadership of Dr. John Bartlett successfully bid for the New York State guidelines contract. As many of you know, John Bartlett has long been one of the leading infectious diseases clinicians in the world, former chief of the infectious diseases division at Hopkins, and chair of the national guidelines panel. John understood that the NYS guidelines were unique in that they targeted primary care clinicians and were an important part of the process to set standards that would be used by payors to guide appropriate reimbursement for care, just as they are anchors to guide measurement of quality of care. The program continues now, following Dr. Bartlett’s retirement, under the leadership of Dr. Chris Hoffmann at Hopkins.
Since 1999, – now 15 years – the Hopkins team has developed over 100 guidelines. They work behind the scenes, diligently and always professionally managing committees, managing physicians, managing AI managers, managing external expert peer reviewers, managing documents, – some drafts well-written and some horribly written – conducting research and designing documents – as well as supporting the hivguidelines.org website where all of our clinical guidelines are posted.
The Hopkins team has managed committees of experts who have developed guidelines not only for adults and children with HIV, but also has supported panels focusing on mental health, substance use, integrating prevention into care, women’s health, oral health care, pharmacy, PrEP and an executive steering committee. Most recently, the program has supported a panel to develop guidelines for hepatitis C mono-infection and will soon be supporting new guidelines for sexual health for MSM. Each guideline is supported by consensus, rated as well based on strength of evidence and then packaged into a formalized style for dissemination and posting.
For the past 15 years, the core of the work and its direction was led by Kathleen Cavolo who in her early 20s, took on the role of managing expert physicians with a natural grace and skill that was coupled with an uncanny ability to understand medical information and make complicated issues understandable. We also take a moment to remember Kathleen who sadly died this fall after a very short aggressive illness. Kathleen was the kind of leader who was able to build a team and translate her knowledge and vision into tangible products as she mentored others to learn about guidelines methodology and implement the management processes to deliver understandable, expert clinical guidance to others. Her legacy is being carried further today by the team that is here to receive the 2014 Linda Laubenstein Award, many of whom have been with the program for over a decade, and contribute the dedicated professionalism that is evident to anyone who reads the guidelines produced by the program. Dr. Hoffmann could not travel to Albany today, however, we are fortunately joined by four members of the JHU team: Zoe Rush, Jesse Ciekot, Barbara Scissors and Thea Brown. Each member of this team makes distinctive contributions that have been fundamental to the success of the program and which play an unseen and unheard role in supporting the visible clinical work of New York State practitioners.
Please join me in congratulating them – in recognition of their outstanding contribution to New York State through development of guidelines that address the care and treatment of people with HIV in New York that provide a framework for excellence in the clinical care of people living with HIV.
2013
Yvette Calderon, MD, MS
Dr. Yvette Calderon has brought an intensity of commitment to efforts to improve HIV testing and prevention in New York City. A graduate of Brown University, Dr. Calderon completed medical school at Albert Einstein, in the Bronx, in 1990. She served as chief resident in Emergency Medicine at Jacobi Medical Center, and after completing her residency, became a full-time faculty member in Emergency Medicine at Jacobi, where she has continued to practice. Since 2011, Dr. Calderon has also served as the Associate Dean of the Office of Diversity Enhancement at Albert Einstein College of Medicine. In addition to these appointments, Dr. Calderon has been actively involved in, and has published on a broad array of research projects on topics that reflect her experiences in the emergency department of an urban public hospital.
In addition to her academic career, Dr. Calderon has been noteworthy for her commitment to the Bronx community, and underrepresented minorities in medicine, and has worked to develop health policies that can be used to improve the health of Hispanic communities.
Of particular note to us, Dr. Calderon has worked to study HIV testing and education in underserved communities utilizing emergency departments, working particularly to engage adolescents and young adults in HIV prevention efforts. She has conducted research that has successfully extended HIV testing to non-traditional areas, and the results of one 26-month study concluded that a video-assisted rapid HIV testing program, even a program located at a busy city hospital emergency department, can effectively test a high volume of patients, successfully link those who test positive to medical care, and provide education and prevention messages to all who test.
Daniel J. Egan, MD, FACEP
Dr. Daniel Egan graduated from Mount Sinai School of Medicine in New York City in 2002. After working for a time in Boston, he moved first to the Emergency Department at St. Vincent’s and then to St. Luke’s Roosevelt Hospital in NYC. He is currently the attending physician in the Department of Emergency Medicine at NYU Langone Medical Center in Lower Manhattan, and serves as the Associate Program Director of the Emergency Medicine Residency Program at NYU School of Medicine.
Dr. Egan has been active in departmental and medical education activities; he is not only a teacher, but has written about improving several aspects of the medical education experience, and has published extensively on various aspects of emergency medicine, including several papers related to HIV testing in EDs and use of HIV post-exposure prophylaxis.
Dr. Egan has addressed the issue of incorporating an HIV testing program from the point of view of the institution, the ED staff, and the patient. His efforts to establish a successful HIV testing and linkage to care program at St. Luke’s Roosevelt (the ninth busiest emergency department in the United States) show a commitment to continuous improvement, as he worked proactively over a period of several years to refine the ED process, to increase those who are tested, and to improve the effectiveness of linking patients to care. He has explored several strategies in order to find a solution that works for both busy staff as well as patients.
In his relatively short career to date, Dr. Egan has made a significant impact on improving the model for HIV testing in the context of emergency medicine, engaging patients who would otherwise remain unaware of their status.
William M. Valenti, MD, FIDSA
Few other clinicians in New York State have played such an important role in working to address HIV/AIDS as Dr. Valenti has during his career. Beginning in the early 1980s, at a time when there was essentially no treatment for HIV, Dr. Valenti has been actively addressing HIV as a clinician, educator, researcher and policy advocate.
A graduate of the Medical College of Wisconsin, Dr. Valenti, an infectious disease internist, has practiced in Rochester, New York throughout his career. He serves as Clinical Associate Professor of Medicine at the University of Rochester School of Medicine and Dentistry, where he has taught since 1975. The topics he has addressed as an instructor range from human sexuality to infection control implementation. In 1989, he was cofounder and the first medical director of Community Health Network, which is now known as Trillium Health. In addition to his clinical duties there, he also serves as senior vice president for organizational advancement.
A true pioneer, Dr. Valenti has been ahead of the curve on many topics related to HIV care that other practitioners are only now beginning to implement—distinct LGBT health care, the need for care coordination, the importance of health literacy, an emphasis on quality of care standards. Early in the epidemic, he recognized the importance of expanding HIV testing methods. In addition to all of these activities, Dr. Valenti has long been involved in the policy aspect of HIV and serves as the chair of the infectious diseases subcommittee of the Medical Society of the State of New York (MSSNY), an organization that represents the interests of patients and physicians in an ongoing effort to ensure quality health care services for all New Yorkers.
2012
Jeffrey M. Birnbaum, MD, MPH
The Linda Laubenstein Award honors a clinician from NYS, who, in addition to providing the highest quality clinical care, is also distinguished by a compassionate manner towards patients. These qualities have been exemplified in the work of Dr. Jeffrey Birnbaum, the 2012 recipient of the Laubenstein Award for HIV Clinical Excellence. Throughout his entire career, Jeff Birnbaum has been committed to addressing the needs of young people with HIV and those at risk.
Dr. Birnbaum attended medical school at SUNY Downstate in Brooklyn, completing his pediatric residency there between 1986-89; he also earned an MPH from Columbia in 1991. Dr. Birnbaum is the director of the Health Education Alternatives for Teens (HEAT) program, which focuses on the special needs of youth infected or at risk of becoming infected with HIV. HEAT is a comprehensive care program offering a full range of medical, mental health, supportive and prevention services. Between 2006-12, he was program director for the Family, Adolescents and Children’s Experience at SUNY (FACES) network, working with vulnerable patients in Brooklyn.
Dr. Birnbaum also serves as Associate Professor of Clinical Pediatrics as well as of Preventive Medicine at Downstate Medical School. His research has been focused on the topics of risk behavior in adolescents, improving medical adherence, and developing prevention protocols. Dr. Birnbaum has been an active leader in the AIDS Institute’s clinical guidelines program since 2000, and was Chair of the Pediatric Guidelines Committee between 2003-2005. He continues to contribute his knowledge and expertise on adolescent treatment issues to the program.
Dr. Birnbaum has taken a unified approach in his commitment to excellent patient care, education, research, and community health, by improving the care provided to adolescents with HIV. Through his clinical practice, teaching, and research efforts, he ensures that a wider audience benefits from his efforts.
2002-2011 Awardees
2011
Roberto B. Corales, DO
Roberto Corales serves as the Chief Medical Officer and Vice President of AIDS Care in Rochester, NY, and he has been working with HIV patients in that community for over ten years. Dr. Corales received his medical training at Michigan State University, completed his residency at Beth Israel Hospital in New York City, followed by an Infectious Disease fellowship at the Cleveland Clinic. He has been consistently involved with clinical research and has been the principal investigator of the AIDS Clinical Trials Group Unit at the University of Rochester.
Dr. Corales has been a leader in addressing the complex needs of his patients and in ensuring that AIDS Care provides a comprehensive center for HIV treatment. He has integrated supportive and clinical services as a treatment home model. His efforts have resulted in publications on a variety of HIV-related topics, and his system-based approach has created a clinic that is consistently responsive to the evolving needs of Rochester patients.
Dr. Corales actively participates in the NYS Quality of Care Advisory Committee, and has implemented multiple improvement activities at AIDS Care. He has recently worked to improve the preventive aspects of clinical practice as an important focus in HIV care. His work combines a public health approach with a commitment to the individual patient.
In addition to medicine, Dr. Corales also trained as a choreographer and dancer, reflecting the creative and innovative approach he brings to his patients. These qualities represent a practitioner who embodies the tradition of clinical excellence recognized by the Linda Laubenstein award.
Peter Gordon, MD
Peter Gordon has been a leader in multiple aspects of clinical care and treatment for patients with HIV throughout his career. He is currently the Medical Director of the Comprehensive HIV Program and Ambulatory Care Network at New York Presbyterian Hospital in NYC, leading a program that provides an integrated team approach to care for a very large population of patients with often specialized needs. Prior to this role, Dr. Gordon served as Medical Director of the Selecthealth Special Needs Plan (SNP) in which his commitment to innovation was shown in developing ways for patients to directly access their medical information. Dr. Gordon received his medical degree from SUNY Stony Brook and completed his residency at Columbia Presbyterian. At Columbia, he has been involved with research efforts and directed the internal medicine residency training program for several years.
For the past 4 years, Dr. Gordon has chaired the NYS Quality of Care Advisory Committee, leading his colleagues in the commitment to ensuring that quality remains part of HIV care considerations for patients throughout the State. He has guided this committee to expand its purview to include areas such as health literacy and coordination of care and has been an articulate champion of the importance of consumer involvement in treatment decisions.
Dr. Gordon has also been an active participant in the NYS Medical Care Criteria Guidelines Committee, bringing expertise and insight to ensure that guidelines meet the needs of even the most challenging patients. As a leader, teacher, and continuous advocate for treatment excellence, Peter Gordon is honored with the 2011 Linda Laubenstein award.
2010
Donna C. Futterman, MD
The Linda Laubenstein awardee for 2010, Dr. Donna Futterman, has been a leader in the treatment of adolescents with HIV since 1989, and currently serves as the Director of the Adolescent AIDS Program, Children’s Hospital at Montefiore Medical Center. Dr. Futterman is also Professor of Clinical Pediatrics at Albert Einstein College of Medicine in the Bronx. As she has since the beginning, Dr. Futterman continues to address the challenges that still exist in the care and treatment of young people with HIV. Dr. Futterman has been committed to social justice issues since before she entered medicine, and her advocacy skills have served her well in promoting the importance of providing clinically excellent comprehensive care for young HIV-infected patients.
Throughout her career, Dr. Futterman has been a national leader in adolescent HIV issues, serving on many policy panels and committees. She has also been involved in international work in South Africa, focusing on youth and newly diagnosed pregnant women. In addition to numerous articles and textbook chapters, Dr. Futterman is the author of Lesbian and Gay Youth: Care and Counseling. Yet she has remained committed to meeting the needs of young HIV patients in the Bronx. Dr. Futterman has long recognized that innovative, targeted strategies are needed to reach and empower at-risk youth.
Dr. Futterman has served on several New York State HIV clinical guidelines committees, working in the 1990s with the late Keith Krasinski. Most recently, she has been the peer reviewer for the NYS guideline addressing the specific treatment issues that are needed to provide ambulatory care for HIV-infected adolescents, applying her clinical expertise to guide others who will care for young patients.
As was this award’s namesake, Linda Laubenstein, Dr. Donna Futterman is not only an excellent clinician, but also provides the committed leadership necessary to address complacency regarding the HIV epidemic and remains an advocate for adolescents and vulnerable populations.
2009
Judith Rees, ACRN, NP
Judy Rees has been the foundation of the SUNY Designated AIDS Care Center in Syracuse, NY for the past 22 years. As the first Nurse Practitioner, and the first NP Program Coordinator for the Syracuse DAC, Judy’s sustained commitment and strong, steady leadership have ensured that the HIV/AIDS program provides outstanding service to PLWHA. Ms. Rees was educated at Mohawk College and received her masters in nursing from Syracuse University. Her duties at SUNY are both clinical and administrative. As a practitioner, Ms. Rees is forward-thinking and experienced in meeting new challenges. She was instrumental in fostering hepatitis C treatment in the DAC and provided the leadership needed to establish anal Pap testing, high-resolution anoscopy and infrared ablation. She has been key in the development and expansion of social work services in the DAC to bett er serve patients with HIV.
As an administrator, Ms. Rees is committed to ensuring that SUNY fulfills its educational mission. She has been largely responsible for the successful recruitment and retention of professional staff and has supported a wide range of staff development activities. She worked to establish “Mini Residency” programs with flexible structures that facilitate a broader range of participation by professional staff. She proactively seeks ways to expand the continuum of care through grants and collaboration. Ms Rees is known by her patients, colleagues, and community for her outstanding commitment to quality care for PLWHA.
Wouter J. Rietsema, MD
Dr. Rietsema is an Infectious Disease specialist who practices at Champlain Valley Physician’s Hospital in Plattsburgh, New York, where he became Medical Director in 1998 and Vice-President of Medical Affairs in 2002. He received his BA from Middlebury College and his medical degree from the University of Connecticut. His post-graduate training extended far beyond New England, as he did his residency in Portland, Oregon, and, as a naval officer, interned and then served as General Medical Officer in the Naval Hospital in San Diego. He is board-certified in Internal Medicine and Infectious Diseases.
For the last 15 years, Dr. Rietsema has been committed to serving the particular needs of PLWHA in the vast North Country of New York State. He created and oversees the outpatient HIV service and practice at Champlain Valley and has provided consultation at the Clinton Correctional Facility in Dannemora. In addition to clinical practice for HIV-positive patients in this area, he also oversees the many dimensions of the comprehensive care that his patients need in both the inpatient and outpatient setting. This rural environment provides great challenges to patient and practitioner alike, as patients must often travel great distances, and there are fewer specialty services available. Dr. Rietsema has been a conscientious voice in ensuring that policies and services continue to address the needs of PLWHA. Dr. Rietsema is actively involved with medical organizations, has published patient case studies, and is committed to ensuring that geography should not be a barrier to excellent HIV care.
Paul A. Stabile, PA-C
After working for 12 years as a meteorologist, Paul Stabile switched careers and returned to school to be trained as a physician’s assistant, committing to working in HIV/AIDS care, which he has been doing since 2001. He now serves as the Director, Clinical Care, at William F Ryan Community Health Center in New York City. His change in career path has been mutually beneficial, for he finds satisfaction in serving PLWHA, and his patients benefit from the advantages of his commitment to excellent care and innovative approaches.
As a clinician and manager, Paul recognizes that additional health needs and social issues challenge his patients, and he provides leadership to address housing assistance, case management, and substance use and mental health treatment. He has worked to integrate these services into his clinic, collaboratively coordinating efforts to keep HIV-positive patients engaged in care. Paul is a systems thinker who has led agency-wide IT and quality initiatives that have become models for other community health centers. His accomplishments at William F Ryan include initiation of treatment of HIV/HCV co-infection so his co-infected patients are able to receive comprehensive care at William F Ryan and do not have to be referred off site. He worked to set up one of the first rapid HIV testing programs in NYC using prevention outreach vans.
Paul Stabile is an active participant in the New York State DOH AIDS Institute’s Quality of Care Advisory Committee, keeping quality improvement efforts in the forefront with his clinic team. His clinical work and his leadership exemplify the outstanding commitment to caring for his patients and the broad commitment to addressing the complex needs of all those in the HIV community.
2008
Judith A. Aberg, MD
Judith Aberg serves as the Director of Virology at Bellevue Hospital Center, is an Associate Professor of Medicine at NYU School of Medicine in New York City, and is the Principal Investigator, AIDS Clinical Trials Unit; remarkably, she has been able to integrate these functions into improving HIV health outcomes, not only for her own patients but for countless other PLWHA in New York State who are affected by her efforts and involvement in treatment and care.
Dr. Aberg has been a leader in HIV clinical care and research for over a decade, securing a national reputation with a combination of advocacy, fierce intelligence, and commitment. Her experiences in research and data management have augmented her engagement in treatment issues. She has been a firm advocate for using evidence to support decision-making, in the context of both guidelines and quality measures, whether addressing population-based treatment or that of an individual patient. Her strong voice and persistence have led to productive outcomes.
As an active participant in the AIDS Institute’s guidelines committee for the care of HIV-infected adults, Dr. Aberg has been able to balance the detail of guidelines recommendations with the larger context of patient care. She has written guidelines on mycobacterial infections and ARV therapy. She has the ability to recognize how guidelines are practiced in an active clinical environment and can therefore shape the discussion by references to real case scenarios. Her input challenges her colleagues to consider other opinions and viewpoints, generating thoughtful discussion and reconsideration of policies and guidelines.
Dr. Aberg has written extensively about a wide range of topics in HIV care, including opportunistic infections and the effects of ARV medications. She has lectured on AIDS topics at venues around the world. On the national scene, Dr. Aberg is Chair of the Primary Care of HIV guidelines committee of the Infectious Disease Society of America and a member of the DHHS working group for guidelines on the therapy of HIV-Related Opportunistic Infections. She also serves as co-chair of the NCQA/AMA/HRSA/HIVMA combined performance measures panel.
Passionate as an instructor, she is actively involved with clinical duties and seeing patients, where she is able to apply her expert knowledge of current research. Dr. Judith Aberg is known for her intellectual rigor, her commitment to scientific evidence-based clinical practice, and her excellence in clinical care.
Lester N. Wright, MD, MPH
Lester Wright serves as the Deputy Commissioner and Chief Medical Officer of the New York State Department of Correctional Services, overseeing a system that provides health care for over 61,000 inmate patients in 70 state facilities. Of the patients in his charge, approximately 4,000 are HIV-infected, giving him one of the largest caseload responsibilities in the State. Unlike many of his correctional colleagues, Dr. Wright’s background is varied not only by experience but also by geography. He has been involved in academic practice and currently serves as a senior lecturer at Columbia University School of Nursing. Dr. Wright has been an advisor in HIV prevention and treatment projects internationally, in both Africa and South America. He has served in the public health divisions of the states of Virginia, Oregon, Kansas, and Delaware, addressing policy matters and directing public health services.
Dr. Wright has been a leader in the New York State correctional system for the past 13 years, and has approached health care in this challenging setting by creating a system for providing quality care to inmates with HIV. He wanted to build a system that would address the treatment issues of those who knew of their diagnosis, and also wanted to be sure that inmates got tested to identify those with HIV who were not aware of their status. He knew that to succeed in bringing quality improvement methods into the correctional health setting he would need to build a quality infrastructure and involve the practitioners in these efforts. He established an innovative clinical education program with Albany Medical Center, which involved transmitting telemedicine sessions on HIV testing, clinical management, hepatitis C, and the special needs of the HIV population throughout the state network of prisons. Dr. Wright showed his commitment to addressing the mental health and substance use needs of his patient population by educating his staff, assuring the availability of services, and establishing special programs to target substance use.
His public health background defined Dr. Wright’s approach to correctional health. He implemented an information system to allow tracking of health information throughout the entire correctional network, one in which patients move around frequently, if involuntarily. This system allowed him to track basic epidemiological data in the prison system and to monitor health outcomes, ensuring that despite their incarcerated status, the health of his patients was a priority and a responsibility.
Lester Wright’s career has been exemplary in his committed service in so many health care arenas. His leadership is often belied by his quiet demeanor and understated achievements, not the least of which has been his accomplishment of providing quality care and service to an underserved population.
2007
Oladipo A. Alao, MD, MPH
Oladipo Alao is Assistant Clinical Professor of Medicine at Columbia University and the HIV Medical Director at Harlem Hospital Center. He completed his residency at Harlem Hospital in 2001 and was an infectious diseases fellow there until 2003. Since 2003, he has overseen the medical and administrative services at Harlem, and leads the quality improvement team. He took on the challenge of leading a clinic that serves a large, complex population of not only adult but also pediatric and adolescent patients. While he has achieved notice for his clinic leadership and training of medical staff, Dr. Alao has also been instrumental in introducing new approaches to caring for patients with HIV/AIDS.
One of these involved introducing a program called Patient Self-Management to help patients with chronic diseases such as HIV/AIDS reach their goals toward self-improvement and a better quality of life. While others may plead being too busy, Dr. Alao and his clinic team participated in a national initiative to improve the ability of patients and their families to undertake the day-to-day management of medication regimens and finding ways to identify and deal with specific health concerns. Harlem Hospital Center began the self-managed support approach in the Family-Centered HIV program. At each visit, the patient reviews goals with the provider, setting an action plan that is behavior-specific and attainable in health improvement terms. Dr. Alao recognized this approach could be successful because it empowers patients who set their own goals, with providers encouraging and reinforcing the process.
Dr. Alao organized an interdisciplinary team approach to improving patient retention, and Harlem was one of the first Health and Hospital Corporation facilities to address this critical issue by linking patient adherence to medical appointments with improved health outcomes. His clinical strategies mark him as a committed physician addressing the needs of HIV patients in the 21st century.
Dr. Alao, a native Nigerian, received his MD degree from the University of Ibadan and his MPH in Epidemiology at Columbia. His publications address a range of topics from causes of chest pain, cryptococcal meningitis, to retention in care. Dr. Alao has been a member of the Quality of Care Advisory Committee at the AIDS Institute and has participated in local, national, and international quality improvement initiatives.
Barbara C. Zeller, MD
Barbara Zeller joined the medical staff of HELP/Project Samaritan (PSI) in 1991, and became medical director shortly after. At that time PSI opened an innovative long term care facility that that incorporated a structured drug treatment program for people living with AIDS. Dr. Zellers’s vision was to provide a compassionate place for healing in which people who felt stigmatized by AIDS and addiction could feel safe and cared for, as a first step in the recovery process. She recognized that sympathetic care and treatment provided hope to patients with this frightening illness, and that with such hope and the tools for change, patients could face the challenges of illness and addiction and create the possibility of regaining dignity and reconciliation with family and community. She fostered the medical team’s understanding that the interdisciplinary care team is critical to a program’s ability to provide appropriate interventions for residents with complex medical, mental health, and social service needs.
Dr. Zeller trained at Columbia University College of Physicians and Surgeons and completed her residency at Roosevelt Hospital’s Internal Medicine Program. Her initial interest in drug and alcohol treatment grew from her experience responding to needs of the underserved that she encountered during her residency. In the late 1970’s she worked to develop Lincoln Hospital’s Detox Program’s first community acupuncture program and School of Acupuncture, among other innovative methods. Her experiences with the devastating effects of HIV/AIDS led her to Project Samaritan and developing a continuum of care for substance users with HIV/AIDS.
Dr. Zeller encouraged clinical research in the long term care setting and was co-investigator on an NIH funded grant addressing the Natural History of Late Stage HIV/AIDS in the Era of HAART. She collaborated with the NYC Department of Health on investigating Influenza A in patients with HIV. Since 2000, Dr. Zeller has chaired the Council of HIV Long Term Care Clinical Directors.
She was involved in the planning group for the Adult Day Health Care Programs for people living with HIV/AIDS, and has utilized her leadership skills in implementing and overseeing the medical component of programs that Project Samaritan opened in the Bronx, Brooklyn and Queens. In 2003, Dr. Zeller spent several months at the Sinikithemba Clinic in Durban, South Africa to provide care and train medical providers who were embarking on their first antiretroviral program. Barbara Zeller’s career has encompassed a wide scope of HIV/AIDS service provision that continues to meet the complete range of medical needs of patients.
Dr. Zeller is a member of the NYS HIV Quality of Care Advisory Committee and is vice-chair of the Women’s Health Care Guidelines Committee of the AIDS Institute.
2006
Elaine J. Abrams, MD
L. Jeanine Bookhardt-Murray, MD
Douglas G. Fish, MD
John AR Grimaldi, MD
2004
Susan Amenechi-Enahoro, MD, MPH, MSc
Dr. Susan Amenechi-Enahoro is recognized for her extraordinary work in serving people living with HIV/AIDS in Brooklyn where she serves as Medical Director of the East New York Adult Day Care Program for Housing Works, Inc. She provides primary health care to homeless people of color who often suffer from concomitant mental illness and/or chemical addiction. She provides empathic, culturally sensitive, excellent care to this extremely hard-to-reach population of HIV patients. She has demonstrated leadership through her determination to include this group in clinical research. Often underrepresented in research studies, communities of color are specifically targeted by Dr. Enahoro for inclusion in clinical trials in order to address the efficacy of interventions that support their access to treatment and care.
Dr. Enahoro studied medicine in Nigeria and obtained her Masters in Public Health from Harvard University, as well as a Masters of Science in Occupational Medicine from the London School of Hygiene and Tropical Medicine. She has been the principal investigator for several HIV clinical projects funded through the New York City HIV Health and Human Services Planning Council, and she has worked in the HIV Clinic at Woodhull Hospital.
Dr. Enahoro’s work in quality improvement has stood out as a superior example of how this methodology can be applied to improve care for people attending adult day health care programs. Her work has been recognized by her peers and selected for presentation at statewide meetings. Her involvement in the statewide Quality of Care Advisory Committee has included important insights that have contributed substantially to the Committee’s work. Susan has dedicated herself to service and truly reflects the ideals honored through the Laubenstein Award.
Marc N. Gourevitch, MD, MPH
Dr. Marc Gourevitch is honored with the Linda Laubenstein Award in recognition of his outstanding achievements and leadership in providing care to people with HIV in New York State, and especially in recognition of his advocacy for comprehensive care to substance users. Following his residency in internal medicine at Bellevue Hospital and fellowship in Epidemiology & Social Medicine at the Albert Einstein College of Medicine, Dr. Gourevitch became an HIV Clinical Scholar to specifically focus on the care of substance users at risk for HIV and those living with HIV. Shortly afterwards, he became the Medical Director of the Substance Abuse Treatment Program at Einstein and the Director of Addiction Medicine and also held academic appointments in the Departments of Medicine, Psychiatry and Epidemiology & Population Health. Currently, he is the Director of the Division of General Internal Medicine and holds a professorship in the Department of Medicine at NYU.
Dr. Gourevitch has directed numerous research studies and published a wide range of papers focusing on the care and treatment of substance users. His academic work and clinical research reflect his commitment to the importance of evidence-based medicine. More importantly, they reflect his commitment to the highest level of care for substance users and to demonstrating the efficacy of treatment in this population. He has consistently advocated for substance users, and fought to ensure that they are not shortchanged in the healthcare system, but rather afforded every opportunity to receive the best possible care.
Dr. Gourevitch has been extremely generous with his time to educate others. He has been a frequent guest lecturer, teaching others how to care for substance users in clinical practice. He has been a proponent of harm reduction methods and substitution therapy and has mentored many others who continue to provide care for substance users with HIV. He willingly agreed to chair the AIDS Institute’s Substance Use Guidelines Committee, leading meetings and editing documents that will be used to promote the quality of care for substance users. He has consistently focused attention on public health issues, including both tuberculosis and hepatitis C, and has helped ensure that these areas were adequately addressed through the state’s quality of care program. For his professional leadership, commitment to the underserved, clinical research and championship of the substance using population, Dr. Gourevitch is awarded the Linda Laubenstein award.
2003
Peter J. Piliero, MD
Dr. Piliero served as the chair of the AIDS Institute’s Medical Care Criteria Committee from 2001 to 2003 and as a committee member from 1999 to 2001. As committee chair he set a new standard for AIDS Institute clinical guidelines committees through his dedication to the job, his ability to find time whenever needed, his rapid responses to questions from the AIDS Institute, other committee members, and the editorial team, and his seemingly limitless fountain of knowledge about HIV. Always concerned for patient safety and comfort as he crafted clinical guidelines, he ensured that the best possible care was reflected in the standards that were set. This commitment to helping each patient live the fullest life possible exemplifies the Laubenstein ideal, and characterizes Dr. Piliero’s dedication and compassion as a clinician.
When Dr. Piliero received this award, he was the Research Director in the Division of HIV Medicine at Albany Medical Center and an Associate Professor of Medicine at Albany Medical College. He was also the Medical Director of the Clinical Pharmacology Studies Unit of the Clinical Research Initiative there. He has published extensively and has been the principal investigator of numerous clinical research studies.
Victoria L Sharp, MD
Dr. Sharp was a member of Medical Care Criteria Committee when it was first established by the AIDS Institute in 1985. At the time, she was the Medical Director of the AIDS Center at Albany Medical Center, setting up the AIDS Program before moving to Manhattan where she took on the task of rebuilding and directing the St. Clare=s Designated AIDS Center Program, the Spellman Center. Exhibiting clear vision and strong leadership, she developed this program into one that stands out as a model, working tirelessly to build systems, obtain grants, and ensure that her patients, including many inmates from the correctional system, would receive good care. She recruited topnotch doctors, developed comprehensive services at the hospital, and established a reputation as a tough and savvy administrator. From there, Dr. Sharp moved to Beth Israel Medical Center, and then to St. Luke’s Roosevelt Hospital Center as the Director of the HIV Center for Comprehensive Care, where she continues to champion care for people living with HIV.
Dr. Sharp serves as Co-Chair of the AIDS Institute’s Physicians Prevention Advisory Committee where she continues to champion the importance of ongoing prevention work in the clinical care setting.
2002
Amneris E Luque, MD
From 1994 to the present, Dr. Amneris Luque has been the Medical Director of the AIDS Center at Strong Memorial Hospital in Rochester, New York, and is an Associate Professor of Medicine at the University of Rochester School of Medicine and Dentistry. Dr. Luque is an outstanding, compassionate HIV/AIDS practitioner, gifted and devoted to both HIV clinical care and clinical education. She is recognized as a consummate clinician and as a role model for setting standards of excellence in the provision of direct patient care.
From 1996-2001, Dr. Luque generously committed her time and in-depth knowledge as a member of the New York State Department of Health AIDS Institute’s Medical Care Criteria Committee (MCCC). Dr. Luque has served as Chair since August 2003. She also served as the Chair of the Committee for the Care of Women with HIV Infection from 2001 to 2003. In addition, she has served as a mentor and preceptor for scholars in the AIDS Institute’s Nicholas A. Rango HIV Clinical Scholars Program. Throughout her years of service, Dr. Luque has been dedicated to staying abreast of the scientific literature about HIV and has been exceptionally talented at translating new developments into practical guidance.
Joseph R Masci, MD
Throughout his career, Dr. Masci has demonstrated extraordinary commitment and leadership in the provision of clinical care for people with HIV infection. Beginning in 1980 at Mount Sinai Medical Center, Dr. Masci cared for some of the earliest reported cases of AIDS in New York City. Having founded the AIDS Program at Elmhurst Hospital Center in 1985, Dr. Masci has directed its growth and operation since that time. He currently serves as the Chief of Medicine, having directed the AIDS Center and Infectious Diseases Division for nearly 20 years.
Dr. Masci has provided years of dedicated service to the New York State Department of Health AIDS Institute’s expert committees. He has been a member of the AIDS Institute’s Medical Care Criteria Committee since 1999 and a member of the Physicians Prevention Advisory Committee since 2002. Dr. Masci has challenged each committee to achieve the utmost in scientifically sound recommendations. Since 1998, he has served on the AIDS Institute’s HIV Quality of Care Advisory Committee, helping to translate clinical practice guidelines into HIV quality of care performance measures. He has provided outstanding service to New York City as the Chair of the Health Services Workgroup, overseeing planning of HIV health services.
Dr. Masci has conducted original clinical research and has published extensively on AIDS-related topics. He is the author of Outpatient Management of HIV Infection, a textbook for clinicians which is used in the United States and around the globe.
1992-2001 Awardees
2000
Gayann Hall, MD
Dr. Hall was the Director of the Infectious Diseases Clinic at Bronx-Lebanon Hospital, a Designated AIDS Center serving over 2,000 patients with HIV/AIDS. She also served as the Clinical Director of the AIDS Institute’s HIV Clinical Education Initiative at Bronx-Lebanon Hospital for over 10 years and also served as the Director of the Nicholas A. Rango HIV Clinical Scholars Program for the hospital. In that capacity, she oversaw and mentored medical residents as they prepared for a career in HIV/AIDS care.
She also served on the Physician Prevention Advisory Committee which developed the New York State Department of Health AIDS Institute’s Clinical Guidelines, HIV & Primary Care: Putting Prevention into Practice. Dr. Hall is widely recognized for her HIV clinical expertise and for her leadership in designing and providing HIV/AIDS clinical education for community-based, primary care settings. She is currently the Medical Director of the HIV/STD/TB Program for the United States Virgin Islands Department of Health.
Neal Rzepkowski, MD
A graduate of SUNY Health Sciences Center, Syracuse, New York, Dr. Rzepkowski has practiced medicine since 1978 and has been board certified in Family Practice since 1981. Since the early 1980′s, he has been actively involved in AIDS care and education on a national level. He served as an emergency room physician in the Emergency Department of Brooks Memorial Hospital, Dunkirk, New York from 1990-1991. Having tested HIV positive in 1985, Dr. Rzepkowski found his career changed dramatically after changes in CDC guidelines were issued in July 1991 for health care workers infected with HIV.
Dr. Rzepkowski has been an outspoken proponent of clinical education for medical personnel and lay people about HIV and AIDS and for fair treatment for people with HIV infection. He devotes much time and energy to improving professional and consumer understanding of HIV transmission, disease progression, and care. Dr. Rzepkowski has demonstrated tremendous courage and tenacity in his effort to confront fear and discrimination related to HIV/AIDS and to counter it with science and reason.
1998/1999
M. Monica Sweeney, MD, MPH
Dr. Sweeney has long served as a tireless advocate for better community health care. She advocates not just treating patients, but treating the needs of communities. Dr. Sweeney’s emphasis is on prevention of disease and empowerment of patients through education. She has a reputation for working effectively with the African-American community and has made great strides in bringing quality health care to the people of Brooklyn. She was an early champion of providing comprehensive, high-quality HIV care in Brooklyn and has remained committed to assuring its continuity.
Stuart L Fischman, DMD
Dr. Fischman retired as Director of Dentistry at the Erie County Medical Center in 1998, but continues to coordinate the oral health care program for the AIDS Designated Care Center at the Erie County Medical Center. Dr. Fischman maintains an active research profile including clinical research regarding the oral manifestations of HIV disease. Dr. Fischman is a member of the AIDS Institute’s Dental Standards of Care Committee.
Since early in the epidemic, Dr. Fischman has been a champion of quality oral health care for people with HIV and AIDS. He provided care at a time when few others would and continues to make an extraordinary contribution to oral health care for people with HIV. Dr. Fischman is now Professor Emeritus of Oral Diagnostic Services at the School of Dental Medicine, State University of New York at Buffalo.
1997
Barbara H. Chaffee, MD, MPH
As an internist deeply connected to the Binghamton community and the Southern Tier of New York State, Dr. Chaffee has a long and distinguished record of personal dedication to the struggle against AIDS. Since 1989, Dr. Chaffee has served in various capacities at the Broome County Health Department including Medical Director of the STD and HIV Clinics and Medical Director of the Broome County Health Department. At the local health department and with United Health Services and the Binghamton Family Care Center, Dr. Chaffee was an important catalyst for HIV treatment services in the region. Traveling extensively in the Southern Tier, Dr. Chaffee helped create access to HIV care in rural areas through clinical education of private physicians.
Dr. Chaffee has an extensive record of service to the New York State Department of Health AIDS Institute. Dr. Chaffee has been the Chair of the HIV Quality of Care Advisory Committee from 1997 until the present. She has served as a member of the Medical Care Criteria Committee since 1997. Dr. Chaffee has been a staunch advocate of integrating the public health model with HIV care.
Ramon A (Gabriel) Torres, MD
During his medical training, Dr. Torres became interested in the health care needs of persons with AIDS and HIV infection. Subsequently, as a primary care physician at a homeless shelter, he cared for hundreds of homeless men and was among the first to note the high prevalence of HIV infection in this population. Dr. Torres was effective in his efforts to bring HIV care to difficult to reach populations, especially immigrants. He achieved national recognition for community-based clinical research regarding the treatment and prevention of HIV and its associated opportunistic infections.
Dr. Torres was a member of the New York State Department of Health AIDS Institute’s Medical Care Criteria Committee and the Quality of Care Committee, and served as the past Chair of the Physicians Prevention Advisory Committee. He has participated on many community, city, state, and federal panels, and served on the boards of many community-based organizations. Dr. Torres exemplifies both the HIV provider with keen insight into the needs of different patient populations, and the active clinical leader who champions the cause of those patients with the greatest needs.
1995/1996
Michael H Grieco, MD, JD
Dr. Grieco was the Director of the AIDS Center Program at St. Luke’s-Roosevelt Hospital Center from 1987 to 1997 and an early leader in establishing comprehensive hospital care for people with AIDS. Dr. Grieco was honored for his leadership role with the AIDS Designated Care Center Program, having served as Co-Chair of the AIDS Institute’s AIDS Center Liaison Committee from 1990 to 1997. Dr. Grieco had an influential role in the creation and refinement of the State’s Medicaid enhanced reimbursement system for HIV care. Dr. Grieco is also commended for the consistent compassion that he has demonstrated in the treatment of people with HIV/AIDS.
Lambert N King, MD, PhD
Dr. King provided invaluable service to the AIDS Designated Care Center Program, having served as Co-Chair of the New York State AIDS Center Liaison Committee from 1990 to 2002. As Medical Director of St. Vincent’s Hospital, he played a key role in supporting the AIDS Center program there. Dr. King also served as a member of the New York State AIDS Advisory Council for several years, a body which advises the State Health Commissioner and Governor on HIV/AIDS policy issues. As a policy-maker, he was particularly influential in ensuring that prisoners have access to HIV care. Dr. King is an exemplary clinical leader, who is sincerely committed to the treatment of people with HIV/AIDS.
1994
Janet Mitchell, MD
Dr. Mitchell’s career reflects her abiding interest in women and AIDS, infant and maternal mortality, adolescent pregnancy, substance-abusing pregnant women, and minority health care. As the Chief of Perinatology, Department of OB/GYN at Harlem Hospital Center in New York City, from 1988 to 1996, Dr. Mitchell recognized the benefits of preventing perinatal HIV transmission. She is also recognized as a pioneer in the care and support of pregnant women with HIV.
1993
Jonathan WM Gold, MD
From 1988 to 1994, Dr. Gold served as the Chair of the New York State Department of Health AIDS Institute’s Medical Care Criteria Committee. His leadership and guidance of the Committee and expert critical review were essential elements in the development of accurate and meaningful state-of-the-art HIV practice guidelines for the clinician. Dr. Gold’s long-term dedicated service is indicative of his exceptional commitment to quality care of patients with HIV/AIDS. Dr. Gold has published extensively on HIV and other human retroviruses, infections in immunocompromised hosts, including those with HIV infection and cancer, and emerging infectious diseases. He has edited two books on HIV infection and AIDS and was the editor of the journal AIDS.
1992
Gary R Burke, MD
On staff at the New York State Department of Health AIDS Institute from 1988 to June 1992, Dr. Burke was Medical Director for more than 2 years, and founded the Office of the Medical Director. In this capacity, he oversaw the development of health care services for people with HIV infection in primary care, hospital services, home care, and long-term care. He initiated a number of AIDS Institute programs, including the HIV Clinical Education Initiative and the Nicholas A. Rango HIV Clinical Scholars Program, that continue to have a significant impact on AIDS education and the treatment of HIV infection. Dr. Burke contributed his medical expertise and vision to the formulation of HIV prevention policies and programs. His efforts have had an important and lasting effect on the continuum of HIV health care services in New York State.